Last updated on: November 4th, 2025 by Fulton Editorial Team
Our feet are remarkable structures that carry us through life—absorbing impact, balancing weight, and supporting every step. Despite their small size, each foot bears three to four times our body weight when we walk, run, or jump. Composed of 26 bones, 30 joints, and over 100 tendons, ligaments, and muscles, the foot works as a finely tuned system for movement and balance. At Fulton, we understand how essential proper foot support is for this foundation—and how one critical ligament, the plantar fascia, plays a key role in keeping you pain-free.
What is it? Definition of Plantar Fasciitis
Plantar Fasciitis is a common yet often misunderstood condition affecting the ligament that supports the arch of your foot—the plantar fascia. This thick, fibrous band connects your heel to your toes, acting like a shock absorber every time you take a step. Dr. De Lucia compares it to a large, flat rubber band that stretches each time you bear weight. Over time, repetitive stress or strain can cause tiny tears or inflammation in the ligament, leading to the sharp heel or arch pain commonly associated with plantar fasciitis.
Symptoms of Plantar Fasciitis
Plantar fasciitis often begins with a sharp, stabbing pain near the heel or arch of the foot—especially during your first steps in the morning or after long periods of sitting or standing. The discomfort usually eases as you move but can return after extended activity, particularly on hard surfaces. This pattern occurs because the plantar fascia tightens while at rest, then suddenly stretches when you stand, causing irritation and inflammation.
Over time, the pain may become more persistent, making walking or standing for long hours difficult. At Fulton, we understand how disruptive this can be. Our arch-support insoles are designed to help relieve this tension by keeping the plantar fascia properly aligned throughout the day, reducing strain, and cushioning every step. With consistent support, you can ease morning stiffness and take pressure off your heels—helping you move more comfortably from your first step to your last.
What Causes Plantar Fasciitis?
When the plantar fascia is overstretched, small tears can develop along the ligament. These microtears often lead to inflammation, stiffness, and sharp pain along the heel or arch. According to Dr. De Lucia, many patients with Plantar Fasciitis have either flat feet or high arches—both of which can strain the plantar fascia. He often sees the condition develop after sudden changes in activity, such as returning to exercise after time off, starting a job that involves prolonged standing or lifting, or wearing shoes without adequate arch support. Over time, repetitive stress without proper recovery can worsen symptoms.
When diagnosing plantar fasciitis, Dr. De Lucia looks for heel or arch pain that’s most severe first thing in the morning or after periods of rest. As patients move throughout the day, the discomfort may gradually lessen. In more severe cases, pain and tightness can extend up through the calf muscles, limiting mobility and making even short walks uncomfortable. Recognizing these early warning signs is key to preventing long-term ligament damage.
Without proper care, plantar fasciitis can worsen over time. Each step may deepen the tears in the ligament, leading to chronic heel pain, gait changes, and even scar tissue buildup. Dr. De Lucia emphasizes that early diagnosis and consistent treatment—especially incorporating arch support and stretching—can make a major difference in recovery. At Fulton, we believe that proactive foot health starts with understanding how your plantar fascia works and supporting it daily with proper alignment and cushioning.
Risk Factors for Plantar Fasciitis
While plantar fasciitis can affect anyone, certain factors make some people more susceptible than others:
- Age (40–60 years). The risk increases as the plantar fascia naturally loses elasticity over time.
- High-impact activities. Running, ballet, or aerobic dance repeatedly strain the heel and arch, contributing to small ligament tears.
- Foot structure and gait. Flat feet, high arches, or abnormal walking patterns can unevenly distribute pressure and overstretch the plantar fascia.
- Occupational strain. Jobs that require prolonged standing or walking—such as teaching, retail, or factory work—can overload the heel and arch.
- Pregnancy-related changes. Hormonal shifts and weight gain can loosen ligaments and place additional pressure on the plantar fascia.
- Unsupportive footwear. Shoes without proper arch support or cushioning increase stress on the fascia. Fulton’s supportive insoles can help reduce this risk by evenly distributing pressure and aligning the foot’s natural arch.
Can Plantar Fasciitis be Cured? Treatments for Plantar Fasciitis
While plantar fasciitis can be painful and persistent, the condition is highly treatable. According to the Cleveland Clinic, nearly 90% of cases improve within 10 months using consistent at-home remedies and supportive footwear. The key is reducing inflammation, resting the plantar fascia, and giving your feet proper support—something Fulton’s insoles are specifically designed to help with.
Short-term, At Home Remedies: Dos and Don'ts
Do:
- Rest and elevate your foot when possible.
- Apply an ice pack (or a bag of frozen peas wrapped in a towel) for 15–20 minutes, every few hours.
- Perform gentle stretching exercises for your calves and arches.
- Try low-impact exercises like swimming or cycling to maintain activity.
- Use supportive shoes or insoles—Fulton’s arch support can help reduce strain on the fascia.
Don't:
- Avoid taking ibuprofen within the first 48 hours of pain onset.
- Limit standing or walking for prolonged periods.
- Skip high heels, flip-flops, or tight, pointy shoes.
- Refrain from walking barefoot on hard surfaces.
Exercises for Plantar Fasciitis Relief
Stretching regularly is one of the most effective ways to ease plantar fascia pain and improve flexibility. At Fulton, we’ve seen that combining consistent stretching with daily arch support delivers the best results. Our custom insoles help stabilize the foot and reinforce the benefits of these exercises, keeping your plantar fascia supported with every step.
1. Achilles Tendon and Plantar Fascia Stretch
Before getting out of bed, loop a towel around the ball of your foot and gently pull toward you while keeping your leg straight. Hold for 30 seconds and repeat three times per foot. This helps warm up the plantar fascia before your first steps of the day, minimizing that sharp morning heel pain.
2. Wall Push (Calf Stretch)
Stand facing a wall with one foot in front of the other. Keep your front knee bent and your back leg straight. Press your hands against the wall and lean forward until you feel a stretch in your back calf. Hold for 30–45 seconds, then relax. Repeat 3–4 times, two or three times per day. Gradually move the back leg farther away from the wall as flexibility improves.
3. Stair Stretch
Stand on a step with your heels hanging slightly off the edge and hold onto a railing for balance. Slowly lower your heels until you feel a gentle stretch in your calves. Hold for 20–60 seconds, then return to your starting position. Repeat up to six times. This stretch helps improve calf flexibility and relieve tension in the plantar fascia.
4. Plantar Fascia Stretch
Sit down and roll your foot gently over a round object such as a tennis ball, frozen water bottle, or rolling pin. Move in multiple directions for 2–3 minutes or until mild discomfort. Repeat twice daily.
Alternatively, cross one foot over your knee, grab your toes, and pull them back toward your body until you feel a stretch along your arch. Hold for 20 seconds, repeating three times per session. Using Fulton insoles alongside these stretches can help maintain proper arch support throughout the day. Learn more about stretching exercises for plantar fasciitis in our full post.
Long-Term Treatment for Chronic Plantar Fasciitis
Long-Term Care for Chronic Plantar Fasciitis
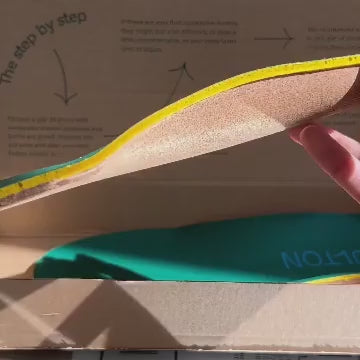
Managing chronic plantar fasciitis requires consistency, support, and patience. One of the most effective long-term solutions is incorporating insoles with proper arch support into your everyday footwear. By supporting your natural foot shape, insoles help reduce tension on the plantar fascia whenever you stand, walk, or run. Over time, this consistent support prevents the ligament from overstretching and promotes healing. Fulton’s custom arch-support insoles are specifically designed for this purpose—molding to your feet for personalized comfort and optimal alignment.
Why Dr. De Lucia Recommends Fulton
Dr. De Lucia recommends Fulton insoles because they provide natural, sustainable arch support that adapts to your unique foot shape. Made from innovative materials, Fulton insoles mold to your feet over time, cushioning pressure points and improving posture. In the context of plantar fasciitis, this alignment is critical—it redistributes pressure evenly across the foot, helping prevent the repetitive strain that causes inflammation and pain.
Other Long-Term Treatments and When to Seek Help
Along with wearing supportive insoles, the Cleveland Clinic recommends daily stretching, gentle foot massages, the use of night splints, and regular icing several times a day to reduce inflammation. If symptoms persist after several months of consistent care, Dr. De Lucia and the Foot and Ankle Surgeons of New York team may recommend medical intervention. They routinely perform surgeries on conditions like Plantar Fasciitis, bunions, metatarsalgia, and achilles tendinitis. For severe cases, Dr. De Lucia notes that Endoscopic Plantar Fascia Release surgery is a highly effective, minimally invasive option that helps reduce inflammation and repair the damaged ligament.
Plantar fasciitis can quickly take a toll on your mobility and quality of life if not addressed early. The good news is that with the right care, recovery is absolutely possible. By combining consistent stretching, proper footwear, and personalized arch support, you can relieve pain and protect your plantar fascia long term. At Fulton, we believe that every step should feel supported—because when your feet are strong and aligned, the rest of your body follows. Learn more about how Fulton insoles can help you move comfortably and confidently.
The Best Insoles for Plantar Fasciitis – Relieving Plantar Fascia Pain
When it comes to relieving plantar fascia pain, the right insole can make all the difference. Fulton’s line of custom arch-support insoles is designed to provide lasting comfort, natural alignment, and reliable relief for every lifestyle. Each product shares Fulton’s signature orthopedic foundation—moldable cork support, deep heel stability, and responsive cushioning—engineered to reduce strain and inflammation in the plantar fascia.
Fulton Products that Address Plantar Fasciitis
- The Classic Insole — Everyday support for sneakers and casual shoes, ideal for reducing plantar fascia strain and maintaining comfort during long hours on your feet.
- The Athletic Insole — Enhanced shock absorption and flexibility designed for active lifestyles, helping runners and athletes recover from repetitive impact stress.
-
The Universal Insole — Slim-fit comfort that discreetly relieves pain in tighter or dress-style footwear without compromising support.
Whether you’re on your feet all day, training for a race, or just looking for dependable comfort, Fulton insoles adapt to your movement and mold to your feet over time. They don’t just cushion your steps—they strengthen the foundation of every stride, helping you move with balance, comfort, and confidence.
About Dr. De Lucia
Dr. De Lucia is dual Board Certified as a Fellow of the American College of Foot and Ankle Surgeons and the American Board of Foot and Ankle Orthopaedics and Medicine. With years of specialized experience in complex adult and pediatric foot and ankle reconstruction, he is recognized for his expertise in both surgical and non-surgical treatments for foot and ankle conditions. As an Honorary Police Surgeon for the New York Police Department, Dr. De Lucia brings a trusted, compassionate approach to helping patients regain mobility and relieve pain. His insight and experience inform Fulton’s mission to make expert-level foot support accessible to everyone.