Updated on February 16 2026, by Libie Motchan
What is metatarsalgia?
Technically, “metatarsalgia is defined as pain in the forefoot under one or more metatarsal heads.” The metatarsals are the five bones that connect the toes to the ankle bones. They connect to the toes at the ball of the foot or forefoot, the padded area between the toes and arch.
This small area repeatedly supports the forces and plantar pressure of your entire body when you stand, walk, or run. Anything that changes weight distribution, deteriorates the support structure of the foot, or increases these forces can potentially contribute to the development of metatarsalgia - pain in the ball of the foot.
What causes metatarsalgia?
There isn’t one single cause of metatarsalgia. It’s a condition that typically develops due to multiple factors. Sometimes it’s biomechanical issues, such as a high arch, flat foot, or development of a bunion. Small changes in your gait (how you walk) can alter shock absorption and general propulsion, putting more pressure on the metatarsals.
In some cases, one of the metatarsals is closer to the ground than the others. Consequently, it absorbs more forces and can become irritated and inflamed. This is considered a static form of metatarsalgia rather than a propulsive form, one related to walking or running.
Chronic illnesses like rheumatoid arthritis, psoriasis, and gout can also contribute to the development of metatarsalgia. Osteoarthritis, for example, can affect a joint near the metatarsals putting more pressure and weight on the metatarsal heads.
Metatarsalgia can also develop after an injury. Overcompensating after a knee, ankle, or unrelated foot injury can change how you distribute weight on the metatarsals, increasing forces and pressure.
Metatarsalgia symptoms
Metatarsalgia usually develops gradually but can sometimes develop suddenly due to an injury. It’s typically felt as a pain in the ball of the foot under one or more of the metatarsals. You may experience:
- Shooting pains
- Sharp pain in the ball of your foot
- A burning sensation
- Aching
- Numbness or tingling in the toes
- Feeling as though there is a small rock under the ball of your foot
Sometimes swelling, bruising, and inflammation are part of the pain. Discomfort gets worse when standing, walking, or running and feels better with rest.
Diagnosing metatarsalgia
Diagnosis usually starts by reporting symptoms to a doctor. After a physical examination, your doctor may order an x-ray to rule out other factors like a stress fracture. If your doctor believes there is a need for closer examination of the soft tissue, the doctor may request an ultrasound or MRI.
After diagnosis, your doctor will work with you to develop a treatment plan. Most treatments begin with conservative, inexpensive at-home treatments. An effective treatment will require consistency until the symptoms stop.
Metatarsalgia treatments
The diverse causes of metatarsalgia have led to an even more diverse range of treatment options. Most medical professionals recommend conservative treatments, such as resting, icing the area, and using over-the-counter pain relievers..
Other conservative treatments include:
- Calf stretches: Tight calf muscles can cause extra strain throughout the ankles and feet. Metatarsalgia exercises include regularly stretching these muscles as a metatarsalgia treatment at home to relieve tension through the calves and feet.
- Metatarsalgia shoes: There aren’t necessarily shoes designed specifically to treat metatarsalgia. However, any shoe that evenly distributes bodyweight across the sole of the foot can be considered the best shoes for metatarsalgia. These types of shoes typically have a wide toe box with a low heel. Keep in mind that the unique shape of each individual’s foot means that different types of shoes might work better for some people than others.
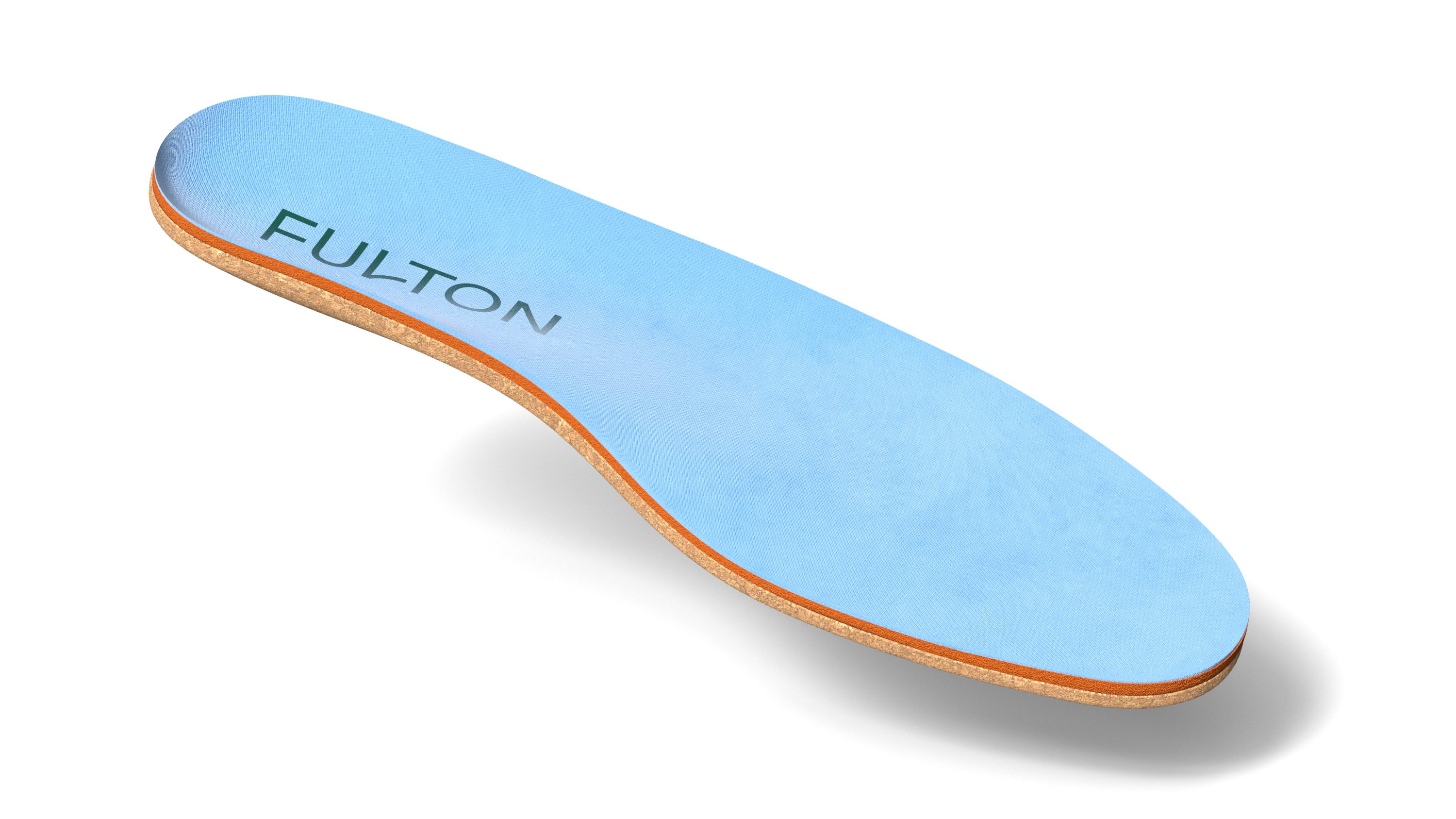
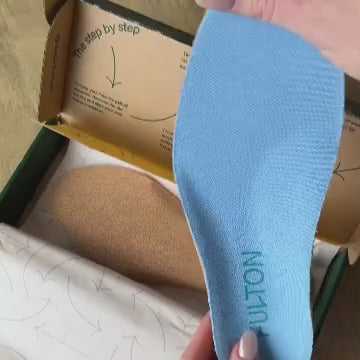
- Metatarsalgia insoles: Insoles, like Fulton Insoles, that support the foot and adapt to the foot’s contours to evenly distribute pressure can treat and prevent metatarsalgia.
- Extra padding: Pads placed in the shoes underneath the forefoot absorb shock. However, they should also help evenly distribute weight.
- Avoid going barefoot: Shoes provide extra shock absorption and pressure relief. Consequently, until metatarsalgia subsides, it’s best to avoid walking barefoot.
- Soaking the feet: Soaking the feet is a simple pain relief method that improves blood flow, try doing this for 20 minutes at the end of the day as needed.
- Callous removal: Callouses can change the pressure distribution on the soles of the feet. Callouses can be removed with a pumice stone after soaking the feet to soften the skin. However, consult a doctor before removing a callous if you have a condition like diabetes that restricts blood flow to the feet.
In some cases, a doctor may recommend surgery of the plantar plate, tendon, or the soft tissues. However, these methods are usually only done after conservative treatments haven’t reduced pain.
Risk factors for metatarsalgia
Anyone can develop metatarsalgia, though there are biomechanical issues and lifestyle choices that put you at higher risk. For example, participation in high-impact sports like running, basketball, and volleyball put high forces and pressure on the forefoot.
Sometimes your biomechanics can make you more susceptible to this type of injury. For example, high arches put more pressure on the heel and forefoot. As a result, walking or running can eventually irritate the metatarsals.
Individuals with a second toe that’s longer than the big toe also tend to develop metatarsalgia more often. Conditions like bunions and hammer toes increase the risk as well.
Wearing high heels put an enormous amount of pressure on the forefoot. Those who wear them frequently may develop forefoot pain over time. Additionally, wearing high heels can cause the calf muscles to shorten, which can further aggravate the condition.
When to see a doctor
Conservative treatments for metatarsalgia, like rest, icing, and over-the-counter pain relievers, can easily be done at home without doctor supervision. Simple changes like replacing worn out shoes or using shoe inserts can bring fast relief as well.
However, if the pain doesn’t improve, seek medical attention if:
- The pain doesn’t improve after trying home treatments
- You experience a sudden increase in foot pain in a period of 20 minutes or less
- You notice a change in the shape of your foot
- The pain prevents you from participating in your regular activities or keeping your knee straight
A doctor can determine if you need to see a podiatrist (foot specialist) or require more in-depth treatment.